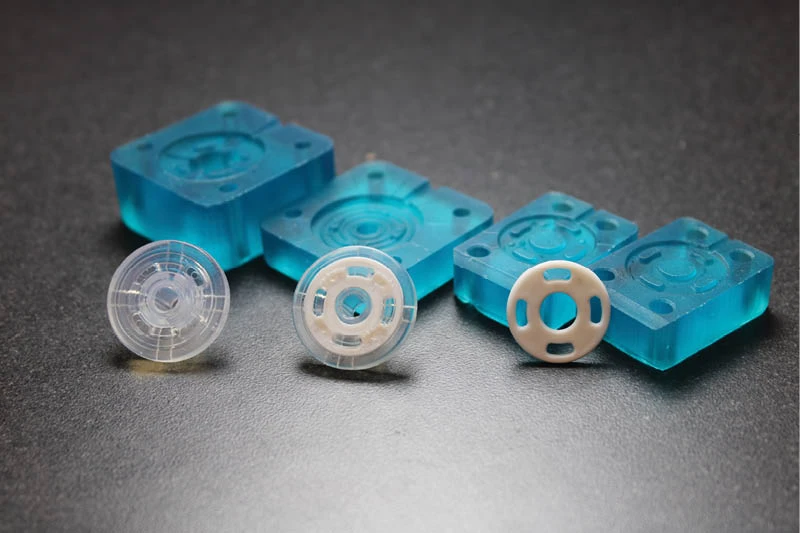
Purdue University photo/Rebecca McElhoe
The vision of Purdue University biomedical engineer Chi Hwan Lee to develop specialized smart soft contact lenses that can accurately measure intraocular pressure (IOP) in a person’s eye could be the latest answer to stopping glaucoma-related blindness.
Lee, the Leslie A. Geddes Associate Professor of Biomedical Engineering in Purdue’s Weldon School of Biomedical Engineering, led a research team that developed new ocular technology to continuously monitor patients’ IOP readings more comfortably and accurately.
The technology serves as another option for eye specialists to identify glaucoma, which, according to the Glaucoma Research Foundation, can steal a person’s vision without early warning signs or pain and affects more than 80 million people worldwide.
The only known modifiable risk factor is lowering a person’s IOP, which is difficult to monitor for long periods of time, particularly during sleep.
While exams can be performed in a specialist’s office and at-home monitoring systems are available, these all have their limitations. For instance, in-office measures are time-consuming, and current at-home technology is difficult to use, is uncomfortable and doesn’t gather sufficient data at the right time periods or over long enough time periods for specialists to appropriately use the information to make optimized treatment decisions.
The new technology is highlighted in a study published in the journal Nature Communications. The study compares Purdue’s technology to the current gold standard and other home monitoring systems and examines how the Purdue technology can gather important IOP measurements for 24-hour cycles, even during sleep.
The technology was developed by a multidisciplinary group of engineers and health care researchers from Purdue’s colleges of Engineering and Veterinary Medicine and the Indiana University School of Optometry.
“The largest increase in IOP often occurs while people are lying down, when overnight IOP is typically 10% to 20% greater than daytime IOP. Vision loss may occur during sleep without the patient noticing it, even if daytime in-clinic or at-home measurements indicate normal IOP,” says Lee, who has a joint appointment in the School of Mechanical Engineering and a courtesy appointment in the School of Materials Engineering.
Lee, who has worked on this technology for six years, specializes in sticktronics, which are sticker-like items that contain electronics or smart technology. His lab develops wearable biomedical devices that can continuously monitor chronic diseases or health conditions in an unobtrusive manner.
Dr. Pete Kollbaum, professor and associate dean for research with the Indiana University School of Optometry and director of the school’s Borish Center for Ophthalmic Research, has worked with Lee since 2019. Kollbaum’s Clinical Optics Research Lab group, which researches contact lens technologies, helped with the human clinical testing and provided feedback for design improvements.
Some of the current wearable tonometers — or devices that measure the pressure inside one’s eyes — are equipped with an integrated circuit chip, which leads to increased thickness and is stiffer than a typical commercial soft contact lens, in many cases causing discomfort for patients. Lee’s version is different.
“To address this unmet need, we developed a unique class of smart soft contact lenses built upon various commercial brands of soft contact lenses for continuous 24-hour IOP monitoring, even during sleep at home,” Lee said.
“Our smart soft contact lenses retain the intrinsic lens features of lens power, biocompatibility, softness, transparency, wettability, oxygen transmissibility and overnight wearability. Having all these features at the same time is crucial to the success of translating the smart soft contact lenses into glaucoma care, but these features are lacking in current wearable ocular tonometers.”
The tonometer on the Purdue-developed contact lens sensor creates a wireless recording that is transmitted to a receiver in a pair of eyeglasses for daytime IOP measurement and a sleep mask for IOP measurement when sleeping.
The complete 24-hour IOP rhythm data can be shared with clinicians remotely via an encrypted server. The tonometer can generate an audible alert for detection of IOP elevation, allowing appropriate action to take place and reducing the need for clinic visits.
“This tonometer is significantly more comfortable than any other type of contact lens sensor we have come across and more comfortable than any currently available commercially available IOP sensor,” Kollbaum said. “This is related to the technology that Lee uses to apply the sensor to the lens, retaining a very thin overall sensor, and to the fact that the lens itself is a time-tested, commercially available lens, leveraging the clinical studies and associated time and money the contact lens manufacturers have spent to assure a comfortable lens.”
Kollbaum said that not only do the specialized contact lenses provide crisp vision, just as any contact lens would, but the technology also expands the benefits for both patients and eye specialists, who have wanted less expensive and more comfortable ways to monitor eye changes for years.
“The eye is a very challenging body part that is even softer, more sensitive and curvilinear when compared to the skin,” Lee said. “We hope our approach can be also tailored for aiding and detecting other chronic ocular diseases and for other functions.”Lee and colleagues have a proposal for additional clinical trials with glaucoma patients who have dry eye diseases or who have had glaucoma surgery. They are also working with Boomerang Ventures, with which Purdue has a partnership, to incorporate the technology into clinical practice.
In addition to Lee and Kollbaum, members of the research team were Shin Ae Park, Seul Ah Lee, Bryan W. Boudouris, Yumin Dai, Keely E. Harris, Bongjoong Kim, Ho Joong Kim, Kyunghun Kim, Hyowon (Hugh) Lee, Kangying Liu, Haesoo Moon, Woohyun Park, Jay V. Shah and Jinyuan Zhang from Purdue; Dawn Meyer from the Indiana University School of Optometry; and Pedro Irazoqui and Brett Collar from Johns Hopkins University.
The technology was disclosed to the Purdue Research Foundation Office of Technology Commercialization (OTC), which has applied for a provisional patent from the U.S. Patent and Trademark Office to protect the intellectual property. For information on licensing opportunities, contact Patrick Finnerty of OTC at pwfinnerty@prf.org about 2021-LEE-69240.
Lee’s work at Weldon School of Biomedical Engineering is just one of many life-changing projects conducted by the biomedical engineering faculty and students. Many of those projects are partnerships among Weldon, health care providers, medical researchers and medical device companies that are key in taking aspects from classes and research labs into clinical settings.
Latest from Today's Medical Developments
- PhD student helps develop medical device for children with congenital heart defects
- Happy New Year
- Best of 2024: #1 Article – 2024 Forecast
- Best of 2024: #1 News – 6 trends impact medtech in 2024
- Best of 2024: #2 Article – Cybersecurity in medical devices
- Best of 2024: #2 News – Miniaturized, implantable multi-sensors device to monitor vessels health
- Best of 2024: #3 Article – Intech Athens deploys ZOLLER tool management system to control tooling inventory
- Best of 2024: #3 News – Avation Medical raises $22 million+