
Photo courtesy of Dassault Systèmes
If ever there was a time to understand the need for speed in the development of new medical treatments, this year of COVID-19 has been it. It is a call to action for all of us to take a hard look at our processes and determine if we are ready for the future. So, to support rapid and sustainable development, Dassault Systèmes and the U.S. Food and Drug Administration (FDA) have extended our collaborative research agreement by 5 years, recognizing the transformative impact of modeling and simulation on public health and patient safety. This extended agreement also supports the 21st Century Cures Act, legislation introduced in 2016 to modernize clinical trials, speed the introduction of new medical technology, and give the FDA greater latitude to recruit support from scientific and technical experts to that end.
Our extended agreement will advance key technologies such as the digital twin for cardiology developed through the Living Heart Project. Hundreds of researchers, cardiologists, and medical device developers are creating and testing highly accurate, personalized models of the human heart. These fully functioning digital replicas leverage Dassault Systèmes’ 3DExperience platform for uniting in vitro, in vivo, and now in silico (in a virtual being) data. They stand in for patients in the design & testing drug therapies and potentially life-saving implants. Because they can be used safely during all phases of development, they accelerate development by lowering the need for surgery and clinical trials, greatly reduce animal testing, and produce zero side effects. Costs fall, long term effects can be considered, lifesaving treatment delivery accelerates, and patient outcomes improve.
In part based on the success collaborating with the FDA, Dassault Systèmes intends to extend virtual twin technology to other body parts.


Meet your twin
Digital (also called virtual) twins are computer-based, 3D models that simulate physical objects. Originally developed for space travel, automakers, for example, can log millions of virtual miles annually in electronic versions of their cars and trucks. Aircraft manufacturers fly digital twins through thunderstorms and land them on virtual runways, while governments use them to design smart, sustainable cities. Often, real-world data flows back to the digital twin to improve the simulation or allow operators to then replicate conditions, such as a virtual check-up.
Digital twins and other advanced simulation tools allow designers and engineers to optimize their products. Engineers can run test scenarios that would otherwise be impossible to replicate and better understand the effects of age, usage, environment, and real-world hazards on their designs. They also make collaboration easier, giving multi-facility or even multinational teams the ability to share ideas and offer suggestions in real-time.
And once the tractor, turbine, ventilator, or refrigerator has been deployed, virtual twins can serve as repositories for Internet of Things (IoT) data from sensors in the field, monitoring life cycle and facilitating service calls while providing critical information for future improvement. The result? Better, safer products, shorter design cycles, and far more efficient manufacturing and maintenance processes.

Leveraging virtual patients
Digital twins emerged as manufacturers wrestled with escalating costs of testing and maintaining new products critical to keep them competitive. Nowhere is this pressure greater than in the medical industry. Global competition, delocalized manufacturing combined with massive costs of clinical trials that suffer from safety concerns, low patient turnout, and yield ambiguous results are just a few of the obstacles facing the medical community. Even trials deemed successful often produce solutions that are less than effective, with costs that can sometimes outstrip their profit. Further, COVID-19 has highlighted an unexpected weakness in the accelerated regulatory process. Through emergency authorization, developers have the authority to treat all patients, eliminating the historic untreated control group due to moral and legal concerns.
A personalized virtual twin of each subject created prior to testing, however, might safely serve the role of the control group. Physicians could collect data from patient wearables and apply it to the twin, identifying trends and potential concerns in real-time. The effects of medications and doses can be simulated before treatment, eliminating guesswork. Virtual patients as a synthetic control group could overcome speed limitations, decreasing cost, trial lengths while outcomes grow more favorable.
And, the technology goes further than that. Innovative doctors are now using digital twins today to develop 3D-printed surgical guides and replicas of organs and blood vessels for training, education, and practice prior to complex surgeries. For life-altering cases such as congenital heart reconstructions, doctors can perform the surgery on the virtual twin of a newborn, to optimize treatment and then go to the OR with much higher certainty. Soon, virtual twins might predict when a hip requires replacement or give trauma surgeons a view of what an accident victim’s knee or skull looked like before the damage.

The twin could then be used to reverse- engineer a precise replacement part. Biomedical engineers could confirm the virtual bone for form, fit, and function before being sent off to CNC machine tools and 3D printers for manufacturing. They could become essential technology as telemedicine emerges as a primary care mechanism, providing a visually informative framework that doctors and patients can understand. This is routinely done for dental replacement, so why stop there?
COVID-19 may have shined a light on the need for speed, but the problem was there. Rising healthcare costs are poised to cripple economies and with aging populations worldwide, it is truly the challenge of our times. Unchecked, this trend will only continue as people live longer, placing additional burdens on governments, insurance providers, and medical practitioners. The stage is set, the technology is ready, and we must rise to this challenge.

The next 10 years
A great deal of work remains before you or I have our own virtual twin, one that our physicians can use to digitally develop and optimize healthcare plans without the traditional poking and prodding and guesswork that we’ve all come to expect. We need to take control and our virtual twin is the way forward. Leading institutions, including the FDA are already incorporating these tools into their practice, gathering critical experience, and setting the stage for the future. Along the way, we are laying the foundation for these types of scenarios to become commonplace.
As with our leadership of The Living Heart Project, Dassault Systèmes is collaborating with others throughout the life sciences value chain. Partners include biopharmaceutical and biotechnology companies, medical device manufacturers, researchers and universities, and governmental regulatory agencies, all of which play a crucial role in determining the future of medicine. We are committed to supporting these companies with innovative tools and technology, pursuing the ultimate goal of a better life for all of us.
Get curated news on YOUR industry.
Enter your email to receive our newsletters.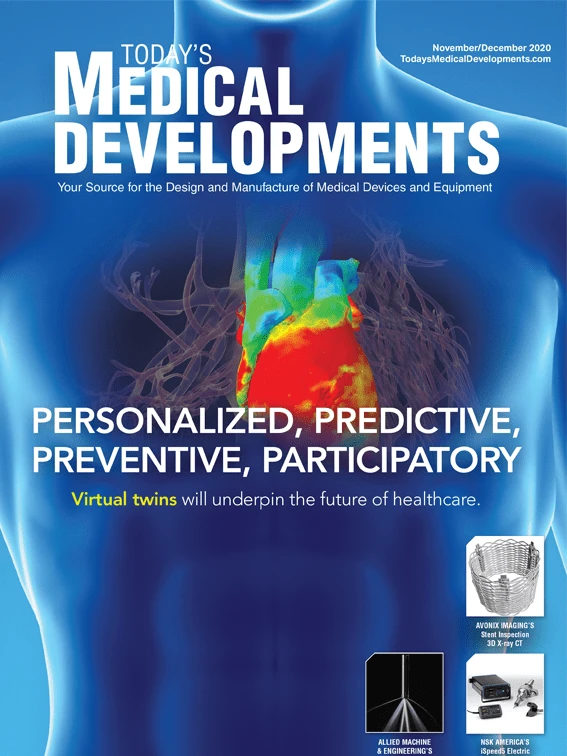
Explore the November December 2020 Issue
Check out more from this issue and find your next story to read.
Latest from Today's Medical Developments
- AdvaMed statement on tariff announcement
- Collets – Not all are created equal
- ENGEL expands production capacities in the Americas; new plant opened in Mexico
- MFI brings fast, high-polishing additive parts finishing to Rapid + TCT 2025
- Teradyne Robotics debuted AI accelerator-powered solutions at NVIDIA GTC 2025
- Measurlabs opens a facility in California
- Sumitomo’s AC9115T & AC9125T – Turning grades for titanium
- #41 Lunch + Learn Podcast - SMW Autoblok






