Researchers at the University of Kentucky and the Georgia Institute of Technology have demonstrated that patches coated on one side with microscopic needles can facilitate transdermal delivery of clinically-relevant doses of a drug that normally cannot pass through the skin.
The study could help advance the use of micro-needles as a painless method for delivering drugs, proteins, DNA and vaccines into the body. The research also found other advantages for the micro-needles, including an ability to produce therapeutic drug levels with lower doses, and lowered production of metabolites that may cause side-effects.
Transdermal drug delivery has proven successful in a number of applications, including pain management, congestive heart failure and hormone replacement. Transdermal administration offers advantages over other delivery techniques, but existing systems can only be used for a narrow range of compounds that easily pass through the skin.
By painlessly punching a series of microscopic holes in the outer layer of skin – known as the stratum corneum – micro-needles promise to expand the range of drugs and vaccines that can be delivered transdermally.
Collaborating with Mark Prausnitz, a professor in the Georgia Tech School of Chemical and Biomolecular Engineering and his Georgia Tech research team, Daniel Wermeling, associate professor of pharmacology in the University of Kentucky's College of Pharmacy, and colleagues Stan Banks, David Hudson and Audra Stinchcomb set out to determine whether micro-needle patches could indeed help deliver useful amounts of drug compounds that otherwise couldn't pass through the skin. As a test compound, they chose the drug naltrexone, a skin-impermeable compound that is used to treat opiate and alcohol addiction.
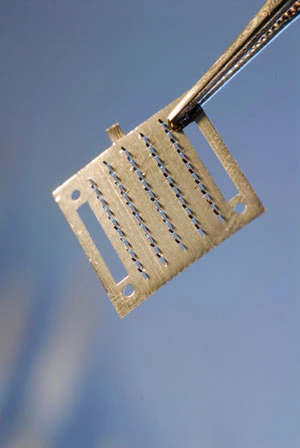
Working with a small group of non-addicted human test subjects, they first prepared a section of skin on each subject's arm by pressing and removing thumbsized patches that contained 50 stainless steel micro-needles, each about 620 microns – about 1/40 of an inch – in length. Next, gel containing naltrexone was applied to the prepared area, which was then covered by a protective dressing.

Micro-needles mounted on an applicator.
The concentration of the drug in each subjects' bloodstream was monitored for 72 hours. The researchers quickly saw levels of the drug reach pharmacologically active concentrations, and those levels remained steady for at least 48 hours in the six test subjects.
Control subjects were treated without the micro-needle preparation prior to application of the naltrexone gel. None of the control subjects had detectable levels of the drug in their bloodstream.
As part of the study, electrical resistance testing of the skin was done on separate subjects to determine how long the pores created by the microneedles remained open. Those tests suggested that drugs could pass through treated skin for at least 48 hours before natural healing processes closed up the tiny punctures.
Micro-needle administration also reduced the amount of drug required to produce therapeutic levels, replacing a 50 mg tablet with 10mg to 12mg of drug in the gel. Use of the micro-needles also produced steady bloodstream levels of the drug, without the initial peak that occurs with oral delivery.

Explore the April 2008 Issue
Check out more from this issue and find your next story to read.
Latest from Today's Medical Developments
- Humanoid robots to become the next US-China battleground
- Air Turbine Technology’s Air Turbine Spindles 601 Series
- Copper nanoparticles could reduce infection risk of implanted medical device
- Renishaw's TEMPUS technology, RenAM 500 metal AM system
- #52 - Manufacturing Matters - Fall 2024 Aerospace Industry Outlook with Richard Aboulafia
- Tariffs threaten small business growth, increase costs across industries
- Feed your brain on your lunch break at our upcoming Lunch + Learn!
- Robotics action plan for Europe





