A new class of small, thin electronic sensors can monitor crucial health parameters after a brain injury or surgery such as temperature and pressure within the skull – and then melt away when they are no longer needed. Eliminating the need for surgery to remove the monitors reduces the risk of infection and hemorrhage.
Similar sensors can also be adapted for post-operative monitoring in other body systems. Leading the research is John A. Rogers, a professor of materials science and engineering at the University of Illinois at Urbana-Champaign; and Wilson Ray, a professor of neurological surgery at the Washington University School of Medicine in St. Louis.
“This is a new class of electronic biomedical implants,” Rogers says. “These kinds of systems have potential across a range of clinical practices where therapeutic or monitoring devices are implanted or ingested, perform a sophisticated function, and then resorb harmlessly into the body after their function is no longer necessary.”
It is crucial to monitor a patient for swelling and pressure on the brain after a traumatic injury or surgery. Current monitoring is bulky and invasive, and the wires restrict the patient’s movement and can complicate physical therapy. The implants’ continuous, hard-wired access to the head also risks allergic reactions, infection, and hemorrhage, and can even exacerbate the inflammation they are monitoring.
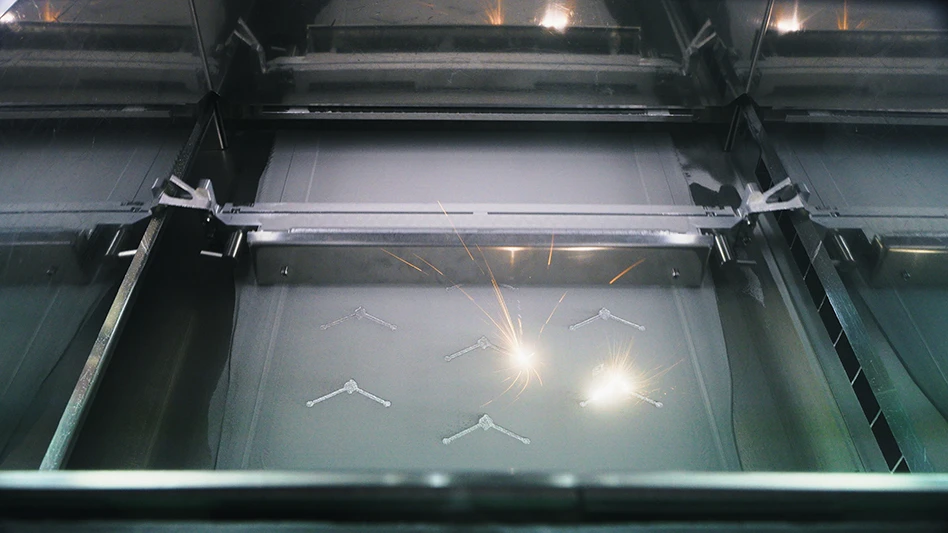
The dissolvable silicon technology developed by Rogers’ group creates sensors smaller than a grain of rice, built on thin sheets of silicon which are naturally biodegradable. The implants are configured to function normally for a few weeks, and then dissolve completely and harmlessly into the body’s own fluids. The silicon platforms are sensitive to clinically relevant pressure levels in the intracranial fluid and have a temperature sensor connected to a wireless transmitter implanted under the skin, on top of the skull.
The Illinois group worked closely with clinical experts in traumatic brain injury at Washington University to implant the sensors in rats, testing for performance and biocompatibility. They found that the temperature and pressure readings from the dissolvable sensors matched conventional monitoring devices for accuracy. The researchers are moving toward human trials for this technology, as well as extending its functionality for other biomedical applications.
“We have established a range of device variations, materials, and measurement capabilities for sensing in other clinical contexts,” Rogers says. “In the near future, we believe that it will be possible to embed therapeutic function, such as electrical simulation or drug delivery, into the same systems while retaining the essential bioresorbable character.”
University of Illinois at Urbana-Champaign
Washington University School of Medicine
Explore the May 2016 Issue
Check out more from this issue and find your next story to read.
Latest from Today's Medical Developments
- HERMES AWARD 2025 – Jury nominates three tech innovations
- Vision Engineering’s EVO Cam HALO
- How to Reduce First Article Inspection Creation Time by 70% to 90% with DISCUS Software
- FANUC America launches new robot tutorial website for all
- Murata Machinery USA’s MT1065EX twin-spindle, CNC turning center
- #40 - Lunch & Learn with Fagor Automation
- Kistler offers service for piezoelectric force sensors and measuring chains
- Creaform’s Pro version of Scan-to-CAD Application Module