When designing a medical product, specific challenges occur during the design process and prototyping stages. Because of the nature of the device, keep these considerations in mind throughout the process, including ease of use and compliance with Food and Drug Administration (FDA) regulations.
Sterilization
Sterilization is crucial for parts of devices that come into contact with a patient. The standard thermometer offers a simple solution: a box containing disposable plastic covers for the thermometer needle. However, not all medical devices have or can have a sterilization feature.
It’s necessary to determine what needs cleaned – camera, tubes, the entire device – when designing the product. There are several questions to consider based on the need of the device, available materials, and sterilization methods:
- Is this easy to dismantle to sterilize?
- Can a single part be removed and replaced after each use?
- During sterilization, are the internal components protected?
- Is there a design flaw that prohibits part sterilization?
Devices used daily require quick and easy cleaning. If the device is too difficult, too expensive, or too time-consuming to clean, buyers will look for alternatives.
Portability
Portable devices are necessary when providing care after disaster strikes or offering basic medical care for those in developing countries. As demand increases for portable devices, designers and manufacturers must fit big capabilities in smaller packages.
Integration
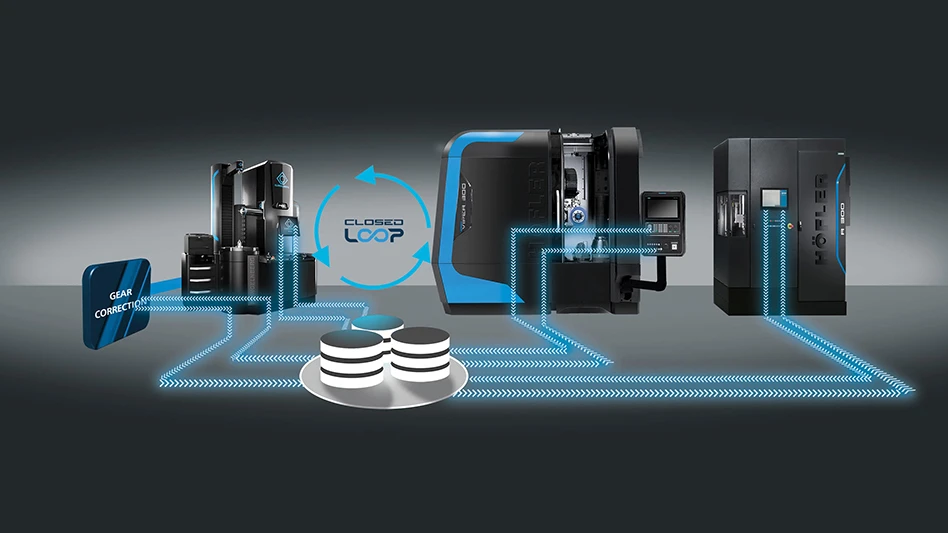
Medical devices need to be designed with synchronization in mind. Capabilities include cyber-secure connection for transferring medical information or imaging to hospital networks or companion devices such as tablets. Also, consider how easy it is to integrate the device with existing technology: can the user implement it, or does it require special knowledge?
This presents a secondary issue since technology changes at an exponential rate. Several laws can predict changes. In 2013, MIT researchers found that of these laws, Moore’s law and Wright’s law were the best predictors. Moore’s law states improvement will double every two years, but the rate is dependent on the technology; Wright’s law states that progress increases with experience.
Keeping these laws in mind, designers should anticipate changes in technology that can render the device useless or momentarily limit its capabilities.
Usability
A device is only as capable as its user. The device may be the most high-tech, highly rated product on the market, but if it’s difficult to use, it’s useless. One way to ensure that the device is usable is to have product testing and feedback sessions so designers can see the device in action. What did users deem difficult, and what visual cues indicated a struggle in using the device?
Usability issues can range from product design to misunderstanding software navigation, and changes may be necessary. With all the changes to increase usability, there may still be human error issues that occur, especially with new, never-before-seen technology.
FDA regulations
The biggest challenge is meeting the FDA Center for Devices and Radiological Health regulations, which include:
- Establishment registration
- Medical device listing
- Premarket notification/approval 510(k) Investigational device exemption
- Quality system regulation
- Labeling requirements
- Medical device reporting
Establishment registration – Any facility that produces and/or distributes medical devices must register with the FDA annually. Additionally, the manufacturer/facility must list the devices created and the devices’ uses.
Medical device listing – Facilities are required to list their devices with the FDA, including manufacturers, re-manufacturers, specification developers, re-packagers, and re-labelers.
Premarket notification /approval 510(k) – Devices requiring a 510(k) require FDA authorization prior to commercial distribution. If the device is high risk, it will need preapproval before going on the market, and if a device requires premarket approval, designs must show clinical data that supports device claims.
Investigational device exemption (IDE) – To secure FDA approval, an IDE is required for the device’s use in a clinical study. If the device poses significant risk, both the FDA and an institutional review board (IRB) must give approval. If the device does not pose significant risk, only the IRB must give approval.
Quality system regulation – The FDA inspects all facilities and aspects of the process to create the devices, including designing, manufacturing, and packaging methods.
Labeling – The device must bear appropriate labels and include companion literature that provides descriptive and informational information about the device.
Medical device reporting – Under the requirements of the FDA’s medical device reporting, all issues with medical devices must be reported, including any malfunctions, serious injury, or death resulting from device use.
Failure to meet these regulations means rejection of the device until in full compliance, so keeping these topics in mind while designing a medical device.
Explore the March 2016 Issue
Check out more from this issue and find your next story to read.
Latest from Today's Medical Developments
- MedTech Innovator welcomes five new industry partners
- First Article Inspection for quality control
- The manufacturing resurgence is here – are you ready?
- Workholding solutions for your business
- ZOLLER events will showcase the company’s cutting-edge innovations
- THINBIT’s MINI GROOVE ‘N TURN Acme threading inserts
- CMMC Roll Out: When Do I Need to Comply? webinar
- Metabolic research uses Siemens gas analyzers to deliver results with 99.9999% resolutions