PHOTO ©GEORGIY | ADOBE STOCK

As we move forward through this COVID-19 crisis, let’s debate what we have done right and what we could do better in future pandemics.
One of the authors of this column recently had an elective procedure that had been delayed three months due to COVID. While the procedure was minimally invasive, the outcome was less than ideal.
At the start of the COVID response, the elective procedure was becoming necessary due to daily health challenges. However, amid forced postponements of these types of surgeries, our patient’s health continued to decline.
The internal pain was severe enough to raise blood pressure to higher levels than previously experienced, highlighted by a hypertensive crisis (190/115) in the middle of the night which led to our patient’s first 911 call and first ride in an ambulance to the local emergency room (made even more uncomfortable as no family member was authorized to accompany). By the time the procedure was finally allowed to take place, our patient was in significant daily pain and having difficulty eating. The good news: our patient is recovering and doing well.
Our patient got off somewhat easy.
Millions of patients worldwide have been severely, negatively impacted by similar COVID crisis choices. The National Cancer Institute predicted that there will be more than 10,000 unnecessary cancer deaths in 2020 due to under-treated cancers in the U.S. alone.
In June, the European Society of Cardiology estimated that more than half of heart attack patients were either not getting care or receiving delayed treatment, increasing cardiology related fatalities.
In orthopedics, GlobalData reported in June that approximately 80% of cases were being delayed or left untreated. Think about the impacts of someone with arthritis being unable to walk and forced into a wheelchair. It makes us wonder if the authorities made the appropriate decisions regarding elective procedures during this pandemic.
While we understand the concern about healthcare staff levels and personal protective equipment (PPE), in hindsight, it’s obvious those fears were misaligned. The reality in most states turned into hospitals laying off healthcare workers due to financial hardship caused by inoperable hospital areas. It’s possible some of these hospitals and care centers may never recover.
Ultimately, COVID crisis management led to a somewhat cruel irony – patients that needed care could not get it because their healthcare practitioners were furloughed, laid off, and unemployed – not because they were unavailable due to COVID. It’s possible that more people will suffer from a lack of access to care (including mental health) than due to COVID.
As experts prepare for the next pandemic, we sincerely hope this sad irony is included in their policy making consideration!

Explore the August 2020 Issue
Check out more from this issue and find your next story to read.
Latest from Today's Medical Developments
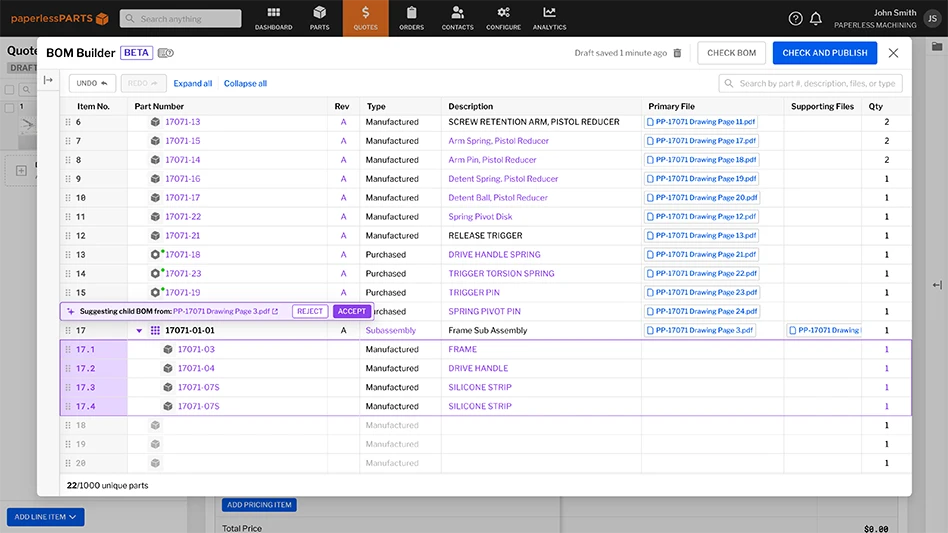
- A 30-year journey through CAM: Insights on simulation technology
- Behringer Saws’ HBE663A Dynamic horizontal bandsaw
- North America's supply chains face sharp decline due to tariffs
- Experience precision: GF Machining Solutions' CUT F Series wire EDM
- Mastering high-temp alloys with Kennametal Inc.
- Integer expands operations in Salem, creating 83 jobs
- Siemens unveils new Teamcenter X: Revolutionizing SaaS PLM for all manufacturers
- 3 Questions with an Expert with Allied Machine & Engineering